Global

Health care workers apploaded in New York | Picture by Vanessa Carvalho/ZUMA Wire/PA Images. All rights reserved
The pandemic has shown how essential care labour is to the functioning of the global economy.
The COVID-19 pandemic has exposed a key truth of human society; at some time or another we all need to be cared for. To visualize this reality, imagine the COVID-19 pandemic is the Titanic and the economy is the iceberg. The collision between the two has revealed what feminist and Marxist scholars have long argued, that below the water line of the formal economy resides social reproduction. This is where essential often invisible or low and unpaid work occurs that supports the structures of the capitalist economy.
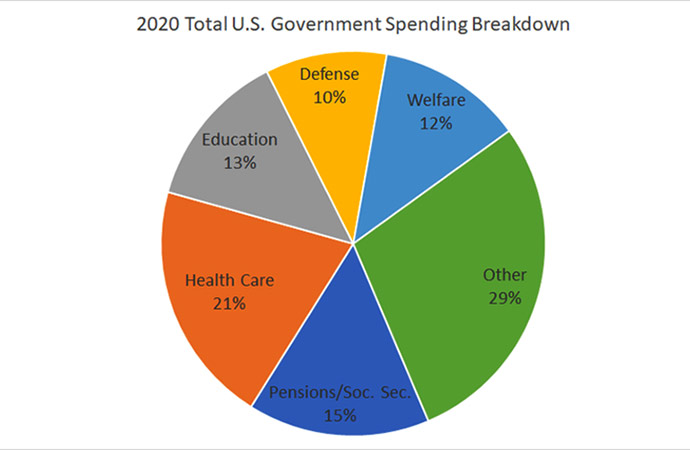
This work of social reproduction allows workers to regenerate themselves (rest, eat and be provided the necessities of life), where those outside of the workforce are cared for and nurtured (the young, the old, the differently abled), and where potential new workers are born, raised and converted into productive members of society and the economy. Research suggests that if this socially reproductive labour were fully accounted for in national calculations, it might increase GDP by anywhere from 15% to 70%.
Women's inclusion in the formal (paid) labour market has increased globally, but men have not taken up much of the double burden of social reproduction tasks. Instead, what has happened in many higher income nations is an increased reliance on often marginalized immigrant women to provide child, elder and other forms of low paid care and domestic service. This process has been captured through the concept of Global Care Chains; the idea that care labour is organized through global chains or connections across different locations that exploit divisions including, but not limited to, gender, ethnicity, class and uneven spatial development. This process has been intensified as governments have withdrawn welfare supports to the young, old and infirm, and families have turned to global care chains to fill in the gaps. This care labour is essential to the functioning of the global economy, but has been devalued and commoditized.
The COVID-19 Titanic, by rendering the submerged mass of the iceberg visible, has exposed how vital these services are to the economy. Suddenly lots of people need looking after. Schools and day cares are closed; children need to be cared for in the home every day. All this 'looking after' has more negative effects on women's employment, especially single mothers. In Canada the March 2020 Labour Force Survey (taken just as COVID -19 public health shut down measures came into place), showed the decline in employment for women aged 25 to 54 was more than twice that of men.
In addition to disruption of child care, COVID-19 has exposed the crisis in elder long term care. In more than half of OECD nations population aging has exceeded the growth in the number of long term care workers. Elder care facilities are some of the worst epicentres of the virus. In France a third of all coronavirus deaths occurred in care homes and in Canada almost a half. Suddenly the terms and conditions of those employed in long term care have become a key concern for the public.
Long term residential care (LTRC) workers are predominately women. Migrant and racialized minorities are overrepresented in the sector. Workers in this sector are low paid, short staffed, mostly part time, who piece together one or more jobs across many facilities. COVID- 19, as with other epidemics before, exposes how these working conditions undermine infection control and make workers and residents vulnerable to infection.
Long term care workers are paid less than hospital workers, but even in hospitals, global care chains funnel workers from lower income nations into core economies. The number of foreign trained doctors, nurses and other health professionals serving the needs of OECD nations' health systems has been on a continued increase over the last decade. On average, across all OECD nations about 30% of doctors and 16% of nurses are foreign trained. Those who engage in international migration to service the needs of OECD nations typically come from lower income countries whose health care systems and health resources are underdeveloped and employment conditions poor.
What might the COVID-19 pandemic mean for these global care chains? The pandemic will result in contradictory processes that might shut down and limit the global mobility of some workers, but, for various reasons (shortages, distributional factors, and the demand for economic and personal security); health systems will continue to rely upon the international mobility of migrant healthcare workers.
We can be optimistic that in the wake of COVID-19 a strong public health system comprised of workers from around the world will be vital to national security; Boris Johnson in London acknowledged this, his life depended on his nurses, Jenny from New Zealand and Luis from Portugal. However, the structural factors that reproduce the devaluation of care work, especially in elder care, will be difficult to shift. Global care chains, and the structural devaluing of feminized and racialized care work they conceptualize, have become a key issue during the COVID-19 pandemic, but they will likely not be deeply altered by it. A deeper transformation in the nature of the economy and society is needed, including how we value the work of social reproduction and care.


















Leave a Comment
Recent Posts
The forensic clean up of the f ...
Much of the coverage centring the surge in Non Performing Loans (NPLs) ...
Hong Kong’s deadliest fire in ...
Hong Kong’s deadliest fire in decades left at least 44 people de ...
False document submission hurts genuine students’ ch ..
The Missing Ingredients for Peace in Palestine
Songs of Hyacinth Boats & Hands: Reading Conversatio ..
Executive Editor Julie Pace on why AP is standing fo ..