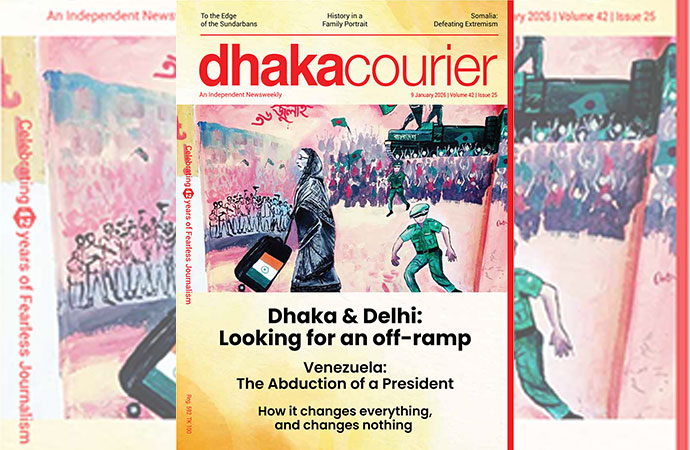
Reportage

DGHS charts show a sharp surge in both cases and deaths from dengue in June.
It mostly passed under the radar, but 2022 was the deadliest year on record for dengue in Bangladesh, where the vector-borne disease with no vaccine has been endemic since 2000. Officially, 269 people died. Despite the first death being recorded as late as June 21, an incredible surge through August to November, unusually late into the year saw the previous highest of 179 (from 2019) easily eclipsed.
The number of cases officially recorded in 2022 was around 62,000. The number of cases in 2019 was 101,354. That means the number of deaths went up by over 50 percent, even as the cases were almost 40 percent down, causing the case fatality rate to spike significantly: a higher proportion of patients catching the disease ended up dead. And already in 2023, we have witnessed the CFR for 2022 eclipsed. After two relatively quiet years in 2020 and 2021, is dengue now getting deadlier?
It is prudent to note however, that according to a paper published by the National Library of Medicine in the US, in 2020-21, as well as the first half of 2022, the true magnitude of dengue infection was possibly "concealed due to severely disrupted healthcare systems to tackle the ongoing COVID-19 crisis." The authors, all Bangladeshi disease specialists, also add that "misdiagnosis or delay in diagnosis of dengue is conceivable because of the similarities in clinical manifestations of these 2 diseases." So we shouldn't make too much of the low numbers during that period.
But there's no escaping the onslaught in 2023, it would seem. At the end of May, the number of cases recorded this year stood close to 2000. It took just 10 days for that to breach the 3000 mark. For much of this past week (till June 15), the number of cases recorded daily topped 200. With the onset of June, deaths have also surged, even more dramatically. Whereas 13 people died in the first five months of the year, that number was easily surpassed in just the first half of the month. As of June 15, 29 people had died of dengue in the country in 2023. The yearly caseload crossed 4000 on that date.
From 2000 to 3000 in ten days, from 3000 to 4000 in five. The onslaught, such that one was anticipated, is well and truly here. The CFR, or case fatality rate for the year stands at 0.71 (approx. 1 in 145 cases end fatally), much higher than the 0.45 (approx. 1 in 220) witnessed in 2022. In 2019 it was 0.17 (1 in 600).
Dreaded Dengue
Yet the truth is there is no specific treatment for dengue fever. Patients should rest, stay hydrated and seek medical advice, according to the WHO. Depending on the clinical manifestations and other circumstances, patients may be sent home, be referred for in-hospital management, or require emergency treatment and urgent referral.
The severe form of dengue causes a fever known as 'breakbone fever', so called because of the severity of muscle spasms and joint pain it causes. That will almost always require medical care by physicians and nurses experienced with the effects and progression of the disease.
Current vaccine options are also very limited. There is currently only one, Dengvaxia, which was developed by the French multinational Sanofi-Pasteur in 2015 and is marketed in 20 countries around the world. But its use is limited by the fact that, when administered to individuals who have never been infected with dengue, it actually increases the risk of developing the more severe version of the disease.
Because of this, it is only recommended for people between the ages of 9 and 45 who have had at least one previous instance of infection. An individual's first infection with dengue is almost always benign, going under the radar in the vast majority of cases. It is any subsequent infection by a different serotype that usually turns severe.In fact the Institute of Epidemiology, Disease Control and Research (IEDCR) director Prof. Tahmina Shirin reported that three of the four known serotypes of dengue - DEN 1, DEN 3 and DEN 4 - were dominating the outbreak in 2022, causing higher fatalities. Previously in Bangladesh two serotypes were known to predominate. Naturally given the epidemiology mentioned above, the addition, and especially prominence of a new serotype would have a significant impact.
The burden in Bangladesh
According to the WHO, dengue is a mosquito-borne viral disease that has rapidly spread to over 100 countries in recent years. Dengue virus is transmitted by female mosquitoes mainly of the species Aedes aegypti and, to a lesser extent, Aedes albopictus. These mosquitoes are also vectors of chikungunya, yellow fever and Zika viruses. Dengue is widespread throughout the tropics, with local variations in risk influenced by climate parameters as well as social and environmental factors.
Dengue causes a wide spectrum of disease. This can range from subclinical disease (people may not know they are even infected) to severe flu-like symptoms in those infected. Although less common, some people develop severe dengue, which can be any number of complications associated with severe bleeding, organ impairment and/or plasma leakage. Severe dengue has a higher risk of death when not managed appropriately.
Severe dengue was first recognised in the 1950s during dengue epidemics in the Philippines and Thailand. Today, severe dengue affects most Asian and Latin American countries and has become a leading cause of hospitalisation and death among children and adults in these regions.
Dengue is caused by a virus of the Flaviviridae family and there are four distinct, but closely related, serotypes of the virus that cause dengue (DENV-1, DENV-2, DENV-3 and DENV-4). Recovery from infection is believed to provide lifelong immunity against that serotype. However, cross-immunity to the other serotypes after recovery is only partial, and temporary. Subsequent infections (secondary infection) by other serotypes increase the risk of developing severe dengue.
Dengue has distinct epidemiological patterns, associated with the four serotypes of the virus. These can co-circulate within a region, and indeed many countries are hyper-endemic for all four serotypes. Dengue has an alarming impact on both human health and the global and national economies. DENV is frequently transported from one place to another by infected travellers; when susceptible vectors are present in these new areas, there is the potential for local transmission to be established, according to the WHO.
In Bangladesh, sporadic cases were first reported in the 1960s and a major outbreak occurred in 2000, with clinical cases reported annually since then. However, the burden of dengue is unclear. Researchers at the Institut Pasteur, an internationally renowned centre for biomedical research, have conducted a study to determine the burden of dengue in Bangladesh and identify key risk factors for infection.
In order to direct precious resources to tackle the virus in the most efficient way, the researchers at the Institut Pasteur, in collaboration with teams at Johns Hopkins University, icddr,b and IEDCR, wanted to know where the risk is the greatest and identify subsets of the population at increased risk. However, this is rarely known, especially in settings with limited surveillance capabilities. Prior to the study, there was essentially no understanding of where dengue virus circulated outside of the capital Dhaka.
"In this context, seroprevalence studies can help. Once infected, individuals develop long-lived antibodies that can be detected by specific tests," explains Henrik Salje, head of the Mathematical Modelling of Infectious Diseases Group at the Institut Pasteur. However, seroprevalence studies are nearly only done in single places, which means their findings are unlikely to be applicable to the wider population. By contrast, in this study, the researchers visited 70 different communities from all around Bangladesh, and invited over 5,000 individuals of all ages to provide blood samples, which were tested for evidence of dengue antibodies. They also asked individuals about themselves, including their age, sex and travel history, and also trapped mosquitoes as part of the study.
The researchers estimated that 24% of the Bangladesh population has been infected by dengue in their lifetime. However, this ranged from 3% in villages in the north of the country to close to 90% in the large urban hubs. They used mathematical models to estimate the number of annual infections and built maps that predicted where risk was concentrated. They estimated that there was an average of 2.4 million infections each year, mainly concentrated in the cities of Dhaka, Chittagong and Khulna. Outside these urban hubs, there was still some exposure to dengue, with risk concentrated in men, who tended to travel more. The main dengue mosquito, Aedes aegypti, was mainly found in urban cities, suggesting its current absence from many rural communities acts as a barrier to "broad nationwide epidemics".
But given that this study dates from 2019, the authorities would be well-advised to replicate precisely such a study, matching its breadth and scale. The sooner we realise the burden of dengue is vital information that citizens could use, the better.
How to fight it?
In one of his appearances on late night television, the dearly departed Mobassher Hossain, architect and urban planner, and man about town, made an impassioned case on our fight against dengue that was impossible to ignore. Appearing on Ekattor TV in October 2022, and confronted with the phenomenal late surge witnessed in the year, he insisted the city corporations were doing it all wrong.
"An Aedes mosquito can fly upto 3 kilometres during its lifetime. But within Dhaka city there are some locations where the city corporations can't even spray insecticide," he said, referring to Pilkhana, the Cantonment and some other restricted zones.
"If we are to really battle dengue, there needs to be a coordinated effort that leaves no stone unturned. Just spraying insecticide, and publishing news on how many litres have been sprayed, and how many people have been fined for allowing larvae on their properties, will not do," Dr Mobassher said, in the sincere voice that was his hallmark.
He even claimed that the method of fogging employed by the city corporations only has the effect of driving mosquitoes that were outdoors, around drains, towards homes searching for shelter, and therefore, even nearer to the people.
Just days after he passed away, in January, Dhaka North City Corporation mayor Atiqul Islam said that he had learned from a trip to Miami, USA (in tropical Florida state, where you get dengue) that the methods employed for eradicating mosquitoes by the municipalities were indeed wrong.
"We have used wrong methods. Mosquitoes were not destroyed, but money was wasted. We want to establish a laboratory for identifying the species of mosquitoes," he said in a statement circulated to the press.
"We want to keep the DNCC mosquito-free through implementing knowledge acquired from Miami." Fair enough. Was there any follow up?
The mayor added that they would organise a virtual meeting with the US authorities engaging Bangladeshi entomologists.
"We will also sketch a work plan so that we can implement that in Dhaka,' he said, adding that they would concentrate on 'a method called larviciding', which would probably mean methods that target the larvae. He said he was done with fogging.
"The weather conditions in Dhaka and Miami are the same. We will succeed as they did. Now there is no time to lag behind," the mayor said. Little did he know.
It's an admirable vision for the future, from the sounds of it. Perhaps it would be implemented, perhaps not. It certainly isn't helping us during the current outbreak.
Scarce alternatives
There is no specific treatment for dengue fever. Patients should rest, stay hydrated and seek medical advice. Depending on the clinical manifestations and other circumstances, patients may be sent home, be referred for in-hospital management, or require emergency treatment and urgent referral. Supportive care such as fever reducers and pain killers can be taken to control the symptoms of muscle aches and pains, and fever.
The best options to treat these symptoms are acetaminophen or paracetamol. NSAIDs (non-steroidal anti-inflammatory drugs), such as ibuprofen and aspirin should be avoided. These anti-inflammatory drugs act by thinning the blood, and in a disease with risk of haemorrhage, blood thinners may exacerbate the prognosis, advises WHO.
For severe dengue, medical care by physicians and nurses experienced with the effects and progression of the disease can save lives - decreasing mortality rates to less than 1% in majority of the countries.
As for existing vaccine options, there is currently only one, which was developed by the French multinational Sanofi-Pasteur in 2015 and is marketed in 20 countries around the world. But its use is limited by the fact that, when administered to individuals who have never been infected with dengue, it actually increases the risk of developing the more severe version of the disease. Because of this, it is only recommended for people between the ages of 9 and 45 who have had at least one previous instance of infection.
In a handful of cities around the world, mosquitoes have been armed with a microscopic weapon against disease. The bacterium Wolbachia pipientis blocks insects' ability to spread fearsome viruses such as dengue, Zika, and chikungunya. Since 2011, researchers have been injecting Wolbachia into the eggs of Aedes aegypti mosquitoes and releasing the hatched insects, which spread this protection to their offspring.
Wolbachia is present in more than 60% of all insects, including dragonflies, butterflies and moths. But the Aedes aegypti mosquito is an anomaly, with no naturally occurring Wolbachia. When the bacterium is introduced into Aedes aegypti eggs, the dengue virus is unable to replicate in the modified mosquitoes that hatch. The exact mechanisms for this are unclear, but some experts suggest that Wolbachia outcompetes the virus for resources such as lipids, or turbocharges the host's immune response, according to a paper published in Nature. Regardless, the Wolbachia-modified mosquito is prevented from spreading dengue through future bites.
There are two approaches to tackling dengue with Wolbachia. The first involves releasing only modified male mosquitoes. Since 2015, this strategy has been successfully adopted in Singapore and Guangzhou, China, and in parts of the United States, such as Miami, Texas and California. Because eggs produced from unmodified females that mate with modified males do not hatch, the number of mosquitoes in the community is greatly reduced.
The second approach, used by some cities in Vietnam, Indonesia, Malaysia, Brazil and Australia, among others, involves releasing modified mosquitoes of both sexes. The infected females pass the bacteria to their offspring. Over time (several months to years, depending on characteristics of the release site), the modified mosquitoes replace the native population.
"The use of Wolbachia as a tool for reducing the capacity of mosquitoes to transmit dengue is a proven technology," says Leo Braack, a vector-control specialist at the University of Pretoria in South Africa, as quoted in Nature. "Its efficacy has been demonstrated in large-scale studies in multiple countries."
According to a paper published in the journal Genetics, dengue fever incidence has been reduced between 40% and 96% in 4 different regions of the world where Wolbachia-infected Aedes aegypti have been established in the field.
"It is not yet clear how sustainable such control programs will prove to be, but there is good reason for optimism," the paper states.
DGHS warning
The Directorate General of Health Services (DGHS) on June 10 issued comprehensive instructions on prevention of dengue infection as the mosquito-borne tropical disease has already increased sharply this year.
According to the data of the DGHS, dengue infection has increased five times since 1 January to 31 May this year. The health directorate has advised to keep clean inside and outside of houses and destroy potential sources of breeding of Aedes mosquito for stopping outbreak of the disease.
It also urged everyone to pay attention to the following issues to combat the outbreak of dengue.
Suspected dengue cases showed some symptoms including 104 degrees body temperature, severe headache, pain behind eyes, pain in body muscles and joints, frequent vomiting, nasal gland swelling and body rash.
Suspected dengue patients with 104 degrees body temperature should visit doctors immediately, the DGHS statement read.
The DGHS also laid emphasis on individual and community alertness to prevent the spread of the dengue disease.
According to the DGHS instruction, Aedes mosquito larvae will die if water accumulated in any container or place in the house and surroundings is cleaned for three consecutive days.
To remove mosquito eggs from used utensils, the utensil should be cleaned by rubbing it with bleaching powder.
Flower tubs, plastic pots, abandoned tires, plastic drums, clay pots, buckets, tin buckets, tin shells or coconut garlands, containers, mats, battery cells should be kept clean as Aedes mosquitoes lay their eggs on those.
Unused water containers must be destroyed or kept upside down to prevent water from accumulating, mosquito nets must be used during the day or when sleeping at day and night.


















Leave a Comment
Recent Posts
Remembering Kalidas Karmakar ( ...
The art world remembers Kalidas Karmakar, a visionary whose creativity ...
An Evening with Shishir Bhatta ...
Cosmos Art Echo, the artist talk initiative of Gallery Cosmos and Cosm ...
Myanmar denies genocide, calls Rohingya crackdown co ..
Yes, of course
Earth’s average temperature last year hovered among ..
Bangladesh and Singapore: A Tale of Two Nations